Sleep Disorders & Treatments
Our sleep studies can diagnose and help treat sleep apnea and other sleep disorders
Get control of your health and life by diagnosing and treating your sleep disorder.
Obstructive Sleep Apnoea (OSA)
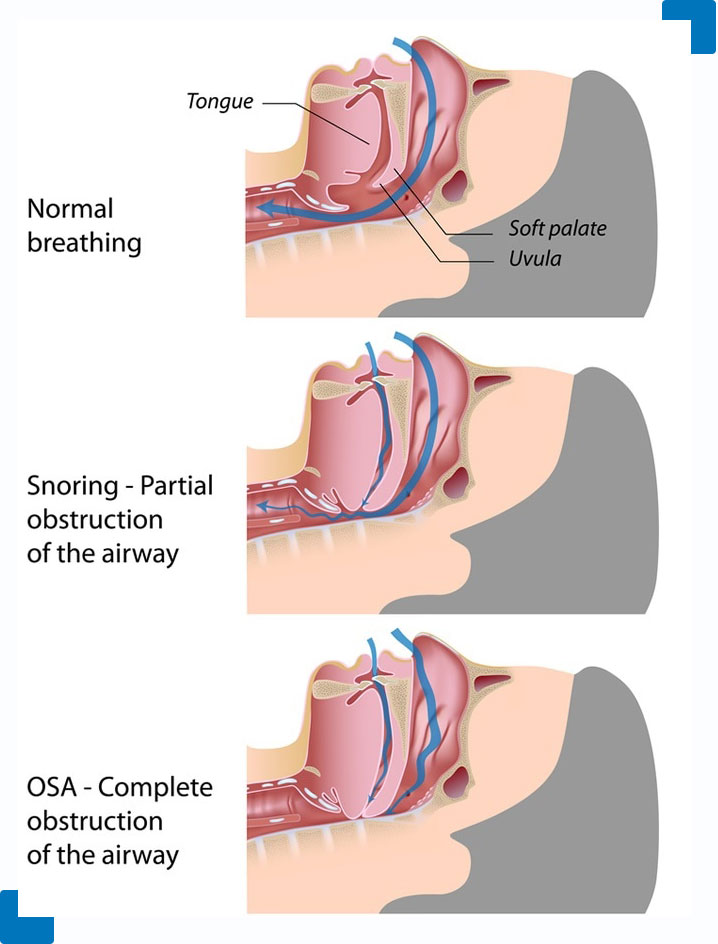
The most common sleep disorder, obstructive sleep apnoea is characterised by repetitive upper airway narrowing or total collapse and is often associated with snoring, decreases in blood oxygen levels and sleep disruption (‘micro-arousals’). There is a wide range of severity from occasional pauses in breathing to hundreds of times in a night and from a few seconds at a time up to minutes at a time of reduced or totally ceased breathing.
Many people are unaware of their obstructive sleep apnoea and report sleeping straight through the night but wake feeling ‘hungover’, however partners of people with sleep apnea will often notice them stopping breathing at night and find themselves counting how long they stop breathing for and waiting anxiously for them to start up again. Sometimes, partners of people with obstructive sleep apnoea will motivate them to consult their doctor because of the major disruption that snoring causes them.
Many people are unaware of their obstructive sleep apnoea and report sleeping straight through the night but wake feeling ‘hungover’, however partners of people with sleep apnea will often notice them stopping breathing at night and find themselves counting how long they stop breathing for and waiting anxiously for them to start up again. Sometimes, partners of people with obstructive sleep apnoea will motivate them to consult their doctor because of the major disruption that snoring causes them.
Typical symptoms are waking un-refreshed, morning headaches, waking with a dry mouth, excessive daytime sleepiness (eg when doing relaxed or repetitive activities), difficulty concentrating or memory problems, mood changes such as irritability or depression, and decreased libido and/or impotence. The milder form can still be associated with snoring, sleep disruption and excessive daytime sleepiness. In its most severe form it is additionally associated with prolonged decreases in blood oxygen that can reach very severe levels with huge strain on the heart, brain and other organs.
Obstructive sleep apnoea can occur at any age, but risk factors for having obstructive sleep apnoea and for having more severe forms of the condition include: older age, male gender, being overweight, severe snoring, having a family history of obstructive sleep apnoea or severe snoring, and post-menopause in women.
The gold standard treatment for obstructive sleep apnoea and particularly its severe forms is Continuous Positive Airway Pressure (CPAP). This therapy involves delivery of air pressure from and air pump to the upper airway through a sealed mask which covers either the nose or both the nose and mouth. By delivering air into a sealed mask, an ‘air splint’ is created in the upper airway which acts to prevent it from collapsing. This relatively simple mechanical therapy is highly effective in eliminating snoring and obstructive sleep apnoea and improving daytime symptoms such as excessive tiredness. The main limiting factor with CPAP therapy is compliance. Because it is a permanent treatment and has to be worn every night and for some people takes some persistence but for the most the motivation to persist with therapy is how good it makes them feel. For this reason, it is extremely important that you get all the support and information you need in the first stages of adjusting to CPAP and an overnight stay Southern Sleep can provide this. The proper support, proper mask fit and accessories such as humidification and a chinstrap will maximise the effectiveness and comfort of therapy and increase the chance of long term compliance. A CPAP supplier can also provide a great deal of information and support.
Other treatments have been shown to have shown to be effective particularly for mild to moderate sleep apnoea, but with more variable success in the more severe forms. Surgery of the upper airway conducted by and ENT surgeon, which tightens and reduces the bulk of soft issue at the back of the throat to try and reduce snoring and sleep apnoea. There are also more radical surgical interventions which involve complete realignment of the jaw.
A novel treatment called pillar procedure has been used in treatment of snoring. It involves insertion of a polyester based material in the soft palate to reduced ‘floppiness’ and hence reduce snoring. Evidence is limited, but early results indicate that this procedure is useful for snoring and possibly mild forms of sleep apnoea.
Mandibular advancement splints (MAS) are made by a dentist or orthodontist and worn like a dental plate. They advance the lower jaw forward to push the tongue way from the airway and reduce the vibrations that cause snoring and airway collapse.
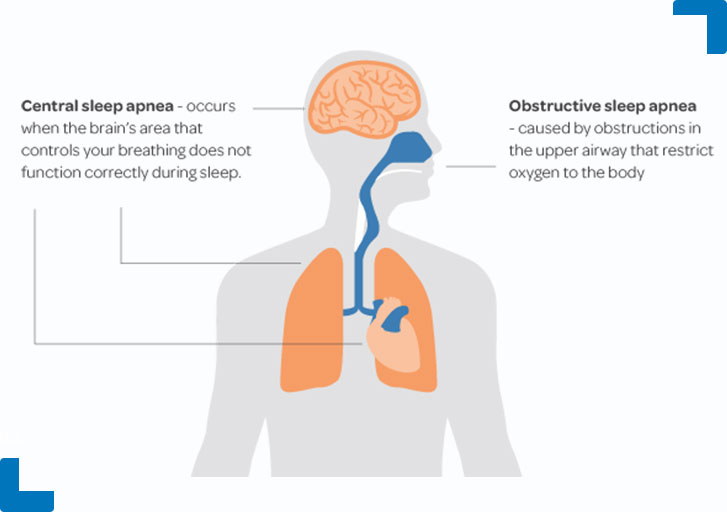
Central Sleep Apnea (CSA)
This much rarer form of sleep apnoea (approximately 5%) occurs as a result of a temporary pause in messages from the brain to the breathing muscles that maintain involuntary breathing when asleep. It can occur because of dysfunction with the brain signals, the muscles or the nerves that send the signals to the muscles.
One type of central apnea more commonly seen and associated with heart conditions is known as Cheyne- Stokes breathing. This is a gradual waxing and waning of breathing effort that is believed to occur because of mis-timing between the brains detection of oxygen and carbon dioxide levels in the blood and the drive of night time breathing which responds to these oxygen and carbon dioxide levels.
CSA can be treated with bilevel types of positive pressure therapy, otherwise called BIPAP or VPAP. This type of treatment is like CPAP in that pressure is non-invasively delivered from a pump to the airway via tubing and a sealed mask, however the machine cyclically delivers a lower pressure on exhalation and higher pressure on inhalation. This acts to ‘breath for you’ and give relief on exhalation. In the setting of CSA, it either takes over and ventilates when there is no breathing effort at all, or amplifies ventilation of the lungs when the person breathing efforts are reduced. It also acts to rests the breathing muscles in between breaths. Special types of these machines are used for Cheyne-Stokes breathing that track the persons wax and wane of breathing effort and deliver a gradually bigger or smaller pressure depending on what is needed.

Restless Legs (RLS) & Periodic Limb Movement Syndromes (PLMS)
These are movement disorders of the limbs that can inhibit a person from falling fall asleep or disrupt sleep continuity. Restless legs is characterised by uncomfortable sensations in the legs and sometimes the arms that can be described anywhere from tingly, restless, crawling, to aching or other pain. People suffering from RLS get the irresistible urge to move their legs about to get relief. The condition becomes particularly prominent when lying in bed at night and makes falling to sleep difficult. The cause is unknown however low iron levels, anaemia, kidney failure, some neurological conditions such as Parkinson’s disease or other conditions that can damage the nerves, pregnancy and caffeine intake have all been associated with RLS.
Treatments are directed at any underlying cause (eg correcting anaemia), and when there is no identified cause therapies for milder cases include exercise, cold or hot packs and reducing dietary caffeine intake. For more severe cases, medications such as benzodiazepines have been used to control symptoms. These medications have a sedating effect to counteract the disruptive impact of the RLS. Opioids such as codeine have also been used.

